By Sarah Russo
Memory is a fundamental component of the human experience that influences each person in a constant, daily manner. Memories enable us to retain our experiences and respond to the constant stimulus we’ve absorbed. There’s much left to learn about the ways we process memories and for what reasons. Active research into these topics may help us to uncover new insight on the brain and methods to treating memory-related ailments.
When memory recall begins to fade, it can have a grave impact on the lives of those affected and their loved ones. Health conditions relating to memory are complex and not fully understood. The general term dementia is applied to a group of symptoms that negatively impact memory. Every three seconds, someone in the world develops dementia. There are an estimated 55 million people worldwide living with memory related illnesses (as per 2020 statistics). That number is projected to double in the next 20 years.1,2
Dementia can also incorporate Alzheimer disease, but the latter is more specific. Alzheimer disease (AD) slowly causes impairment in cognitive function and memory due to its progression in the brain. There is no cure and the exact cause is unknown. The process begins years before the first symptoms are expressed. Brain proteins stop functioning normally at a basic level. This disrupts the normal functions of neurons. As a result, they become damaged, lose connections to one another, and die. The destruction most commonly starts parts of the brain controlling memory. Then neuron loss spreads to other brain regions. Once the disease has progressed to later stages, the brain has considerably atrophied.3,4
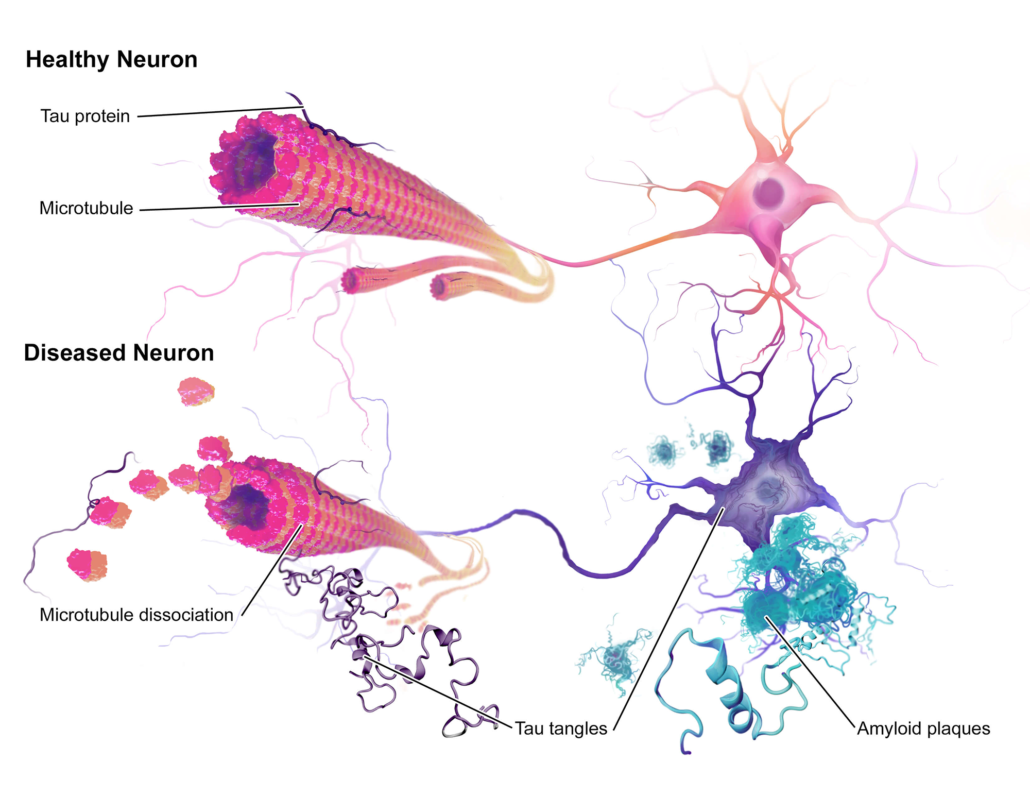
Researchers trying to understand the cause of AD are focused on the role of two protein complexes: amyloid plaques and neurofibrillary tangles. Amyloid plaques are found in between neurons. Plaques emerge when beta-amyloid fragments cluster together, which has a toxic effect on neurons and disrupts the communication between cells.3,4
Tau proteins play a part in a neuron’s internal support and transport system. These proteins carry nutrients and other essential materials. Neurofibrillary tangles develop when tau proteins change shape and organize themselves into structures. These tangles disrupt the transport system and are toxic to cells. Current methods for treatment are generally focused on slowing or stopping the progression of plaques and tangles.3,4
Issues with standard treatment options
The symptoms of AD are complex and can vary in severity from patient to patient. Most people eventually end up with some degree of neuropsychiatric symptoms, which are considered to be a hallmark of the disease. This often causes distress both to patients and caregivers. Current treatments cannot stop or reverse the progression of the disease. They may, however, slow it down a bit. Non-pharmacological methods such as music, melatonin, and behavioral intervention are recommended as a first line treatment. While these may help to some degree, they are usually not completely effective.5
There are four FDA-approved pharmaceuticals approved in the USA to treat memory loss: galantamine, donepezil, tacrine and rivastigmine. These four medications have mild benefits on a temporary basis. They are designed to increase the amount of acetylcholine, the memory molecule in the brain that becomes depleted in AD. However, none of these medications show strong evidence of efficacy and are only for short-term use. Acetylcholinesterase inhibitors also come with common side effects, such as nausea, vomiting, diarrhea, weight loss, muscle cramps, insomnia, fainting, confusion… And the list goes on.4,6
In regards to mental health distress, no current pharmacotherapy is approved for agitation in AD. Commonly used antipsychotics, anxiolytics, antidepressants, and hypnotics are often associated with an increased mortality rate. Antipsychotics specifically are not recommended by any medical organization, unless there are no other methods that can be implemented. Their use is heavily regulated in all assisted living facilities.5,7 It is essential to examine alternative treatment options for managing the disease and its associated symptoms. Alzheimer disease requires treatment regimens that affect multiple targets in order to alleviate the multitude of issues associated with the disease.6 There is strong interest in cannabis and the modulation of the endocannabinoids system (ECS) as a prospective area of investigation.
The Role of the ECS
The effects of the ECS on Alzheimer’s disease are likely multifactorial. AD is associated with neuroinflammation, excitotoxicity, and oxidative stress. These parameters are mediated by the ECS. Endocannabinoid function modulates the principal processes of AD during neurodegeneration, where cells of the central nervous system die or fail to work.4
Various research has examined how the endocannabinoid system is involved in the development of AD. For example, analysis has revealed shifts in the ECS of those with the disease. This includes the observation that CB2 receptor expression is noticeably increased in specific brain regions while CB1 receptor expression is decreased. In addition, there is increased CB2 receptor expression in and around amyloid plaques, which suggests a correlation between plaque deposition and the ECS.8
The importance of the gut biome should also be noted for AD treatment. The ECS acts as a bridge between the body and its internal bacteria, which includes the brain. Research has indicated a clear connection between gut flora dysbiosis and AD physiopathology. Realigning the intestinal microbiome may help offer innovative perspectives on managing the disease.8
Cannabis and Dementia
Current investigation has reported that cannabis might be useful for reducing some symptoms associated with AD and dementia. Mikhail Kogan, MD has been involved in clinical care of patients with AD for over 10 years and has been advocating for the inclusion of medical cannabis into integrative geriatrics. Integrative geriatrics centers on the patient and uses mainly non-pharmacological approaches to provide medical attention to the elderly. This framework is rooted in lifestyle interventions such as nutrition, movement therapies, and the alignment of mind, body, and spiritual wellness. This enables patients to use pharmaceutical approaches and invasive procedures only when safer options are unavailable or not effective.5
Cannabinoids have long been investigated for their neuroprotective and anti-inflammatory properties. Interest on cannabinoids in dementia stemmed from their ability to reduce build-up of toxic abnormal proteins in the brain in lab and animal studies. Both CBD and THC have the potential to slow or perhaps even stop the degenerative process based on preclinical studies. Synthetic drugs created for these purposes have yet to advance in the clinic.4,9,10 Both CBD and THC has demonstrated the ability to interfere with the production of abnormal toxic matter in the brain of dementia patients. In addition, CBD has shown beneficial effects for patients with agitation, sleep disorders, or eating problems. It has also been found to reverse and prevent the development of cognitive deficits in AD rodent models.4,11
In patients with the more advanced forms of Alzheimer Disease, it’s possible that down-regulating endocannabinoid FAAH (fatty acid amide hydrolase) with THC can have beneficial inhibitory effects. COX-2 inhibition, which regulates the inflammatory process in the body, may also have some benefits. CBDA may have some benefits in this regard.5,6
In clinical research, THC has been shown to decrease nighttime agitation for dementia patients, thereby improving sleep and appetite. In a 1997 clinical study of 15 dementia patients who refused to eat, Marinol® was given which led to increased body-mass index. An open-label 2-week study of six dementia patients in 2006 had improvement in nocturnal motor activity, agitation, appetite, and irritability when taking 2.5 mg of THC once in the evening.12,13 However, a 2015 study of 50 dementia patients failed to show improvement for neuropsychiatric symptoms when taking THC only. The authors noted that the dose of 1.5 mg THC three times per day may be inadequate and higher doses might be required.12,14
Clinical examinations using herbal cannabis have been limited. A whole plant cannabis study was performed by SCC past president Jeff Hergenrather, MD and colleagues in a California nursing home in 2017. Patients were given one of three options administered in tinctures and edibles: a THC-predominant option, CBD-predominant, and THCA. Cannabis preparations were noted to decrease agitation, increase appetite, and improve sleep quality, objective mood, self-mutilation, and pain control. Some patients were also able to take fewer neuroleptic drugs as a result of using cannabis.12,15
There needs to be more investigation on whole plant cannabis preparations and how they may influence specific AD symptoms. Based on the pharmacology of the cannabis plant, the below components may offer benefits that target specific aspects of the disease:
- Agitation: CBD, THC, linalool
- Aggression: THC, CBD, linalool
- Anxiety: THC (low dose), CBD, linalool
- Anorexia: THC
- Psychosis: CBD
- Depression: THC, limonene, CBD
- Insomnia/Restlessness: THC, linalool
- Memory: THC + alpha-pinene
- Neuroprotection: CBD, THC
- Pain: CBD, THC
- Reduced Aβ plaque formation: THC, CBD, THCA16
A Final Note
There is a solid scientific basis for the use of cannabis in treating Alzheimer disease. Cannabis compounds promote the brain’s intrinsic repair mechanisms and have been found to reduce oxidative stress and neuroinflammation. Cannabis may boost mood, soothe agitation, and encourage appetite and weight gain for AD patients. Since dementia and Alzheimer disease are impactful conditions for those affected and their loved ones, more focus should be put on integrative care that incorporates natural approaches with cannabis.
For in depth considerations of the topics of cannabis medicine for Alzheimer disease, you may check out the SCC courses Cannabis in the Management of Neurodegenerative and Movement Disorders (Stacey Kerr, MD) and Cannabis in Geriatrics & Assisted Living (Mikhail Kogan, MD).
This article may not be reprinted without permission.
 Sarah Russo is the Creative Director for the Society of Cannabis Clinicians. She got her degree in Environmental Studies and Social Justice, with a focus on botanical medicine from the Evergreen State College. She is a freelance writer, organizer, consultant, and digital creative with over 13 years of experience in the cannabis and herbal medicine space. She is also the founder of Herbs for the Apocalypse, a graphic novel and passion project aimed at deepening our connection to plant medicine and forging resistance and resilience in trying times.
Sarah Russo is the Creative Director for the Society of Cannabis Clinicians. She got her degree in Environmental Studies and Social Justice, with a focus on botanical medicine from the Evergreen State College. She is a freelance writer, organizer, consultant, and digital creative with over 13 years of experience in the cannabis and herbal medicine space. She is also the founder of Herbs for the Apocalypse, a graphic novel and passion project aimed at deepening our connection to plant medicine and forging resistance and resilience in trying times.
Citations
- Greshko, Michael. (2019). The human memory—facts and information. National Geographic. Accessed on 11/07/2021
- Alzheimer’s Disease International. (2020). Dementia statistics. Accessed on 11/07/2021
- Mayo Clinic Staff. (2021). Alzheimer’s disease – Symptoms and causes. Accessed on 11/07/2021
- Kerr, Stacey. (2021). Cannabis in the Management of Neurodegenerative and Movement Disorders. Society of Cannabis Clinicians Medical Cannabis Clinical Training Module.
- Kogan, Mikhail. (2021). Cannabis in Geriatrics & Assisted Living. Society of Cannabis Clinicians Medical Cannabis Clinical Training Module.
- Rosner, Abbie. (2019). Cannabis For Parkinson’s And Alzheimer’s Diseases -An Interview With Dr. Ethan Russo. Forbes. Accessed on 11/11/2021
- Kales HC, Valenstein M, Kim HM, McCarthy JF, Ganoczy D, Cunningham F, Blow FC. Mortality risk in patients with dementia treated with antipsychotics versus other psychiatric medications. American Journal of Psychiatry. 2007 Oct;164(10):1568-76.
- Seltenrich, Nate. (2021). Alzheimer’s Disease & the Endocannabinoid System. Project CBD. Accessed on 11/11/2021
- Eubanks LM, Rogers CJ, Beuscher IV AE, Koob GF, Olson AJ, Dickerson TJ, Janda KD. A molecular link between the active component of marijuana and Alzheimer’s disease pathology. Molecular pharmaceutics. 2006 Dec 4;3(6):773-7.
- Iuvone T, Esposito G, Esposito R, Santamaria R, Di Rosa M, Izzo AA. Neuroprotective effect of cannabidiol, a non‐psychoactive component from Cannabis sativa, on β‐amyloid‐induced toxicity in PC12 cells. Journal of neurochemistry. 2004 Feb;89(1):134-41.
- Watt G, Karl T. In vivo evidence for therapeutic properties of cannabidiol (CBD) for Alzheimer’s disease. Frontiers in pharmacology. 2017 Feb 3;8:20.
- Russo EB. Cannabis therapeutics and the future of neurology. Frontiers in integrative neuroscience. 2018 Oct 18;12:51.
- Walther S, Mahlberg R, Eichmann U, Kunz D. Delta-9-tetrahydrocannabinol for nighttime agitation in severe dementia. Psychopharmacology. 2006 May;185(4):524-8.
- Ahmed AI, Van Der Marck MA, Van Den Elsen GA, Olde Rikkert MG. Cannabinoids in late‐onset Alzheimer’s disease. Clinical Pharmacology & Therapeutics. 2015 Jun;97(6):597-606.
- Hergenrather J. Cannabis and Dementia. Columbus, OH: Cannabis Expertise. 2017.
- Russo EB, Marcu J. Cannabis pharmacology: the usual suspects and a few promising leads. Advances in pharmacology. 2017 Jan 1;80:67-134.